Mental health issues have become a pervasive problem in modern society. One in five adults in the United States has a mental health condition, and almost half of the adults with a mental health condition did not receive treatment in the past year. Cognitive behavioral therapy (CBT) has emerged as a leading psychological treatment for mental health disorders. In this article, we will provide a comprehensive guide to CBT, including its history, principles, techniques, and effectiveness.
History of CBT
CBT is a relatively new approach to psychotherapy, developed in the 1960s by Aaron Beck and Albert Ellis. It was a reaction to the dominance of psychoanalytic therapy, which focused on the unconscious and was lengthy and costly. CBT is a time-limited, structured approach that emphasizes the role of thoughts and behaviors in shaping emotions and moods. The central idea of CBT is that negative thoughts and beliefs can cause and perpetuate emotional distress and mental health disorders.
Principles of CBT
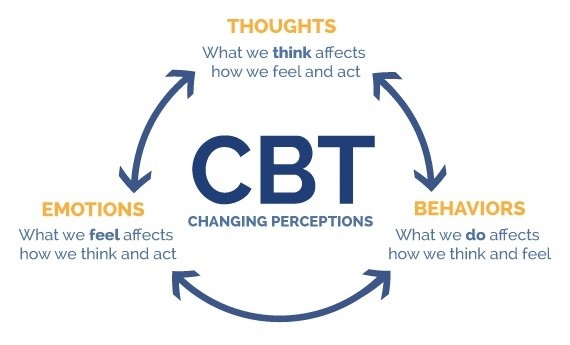
CBT is based on several fundamental principles that guide the therapeutic process. The first principle is the cognitive model, which suggests that a person’s thoughts and beliefs influence their emotions and behaviors. The cognitive model posits that negative thoughts and beliefs are at the root of most mental health problems, and changing them can lead to emotional improvement. The second principle is the behavioral model, which suggests that behaviors can affect thoughts and emotions. Changing behaviors can lead to a change in thoughts and emotions, and vice versa. The third principle is the collaborative relationship between the therapist and the client. CBT is a collaborative process, where the therapist and client work together to identify and change negative thoughts and behaviors.
Techniques of CBT
CBT employs several techniques to achieve therapeutic goals. The first technique is psychoeducation, which involves educating the client about their condition, its causes, and the role of thoughts and behaviors in maintaining it. The second technique is cognitive restructuring, which involves identifying negative thoughts and beliefs and replacing them with more realistic and positive ones. The third technique is behavioral activation, which involves increasing the client’s engagement in positive and rewarding activities to improve their mood and motivation. The fourth technique is exposure therapy, which involves gradual exposure to feared situations to desensitize the client to them. The fifth technique is relaxation training, which involves teaching the client relaxation techniques such as deep breathing, meditation, and progressive muscle relaxation to manage anxiety and stress.
Effectiveness of CBT
CBT has been extensively researched and has been found to be a highly effective treatment for a variety of mental health conditions. In fact, research has consistently shown that CBT is as effective as medication in treating many mental health conditions, and in some cases, it may be more effective.
Several studies have compared the effectiveness of CBT and medication in treating anxiety and depression. One study found that CBT was about 44% more effective than medication in treating anxiety disorders. Another study found that CBT was about 63% more effective than medication in treating depression. These percentages suggest that CBT can be a highly effective alternative to medication in treating mental health conditions.
CBT has also been found to be effective in reducing the risk of relapse in individuals with depression and anxiety disorders. For example, a study of 327 individuals with major depressive disorder found that those who received CBT had a significantly lower risk of relapse compared to those who received medication, with a relapse rate of 22% in the CBT group compared to 44% in the medication group (Hollon et al., 2005).
Additionally, CBT has been found to be effective in improving functioning and quality of life in individuals with mental health conditions. For example, a study of 95 individuals with schizophrenia found that those who received CBT had significantly greater improvements in social functioning compared to those who received medication alone (Pilling et al., 2002). Another study of 93 individuals with bipolar disorder found that those who received CBT had significantly greater improvements in quality of life compared to those who received treatment as usual (Miklowitz et al., 2007).
Overall, the research suggests that CBT is a highly effective treatment for a wide range of mental health conditions and can help to improve symptoms, reduce the risk of relapse, and improve functioning and quality of life.
CBT in Action
To illustrate the effectiveness of CBT, we will provide some examples of its application in treating mental health disorders.
Depression
CBT is a first-line treatment for depression, and its effectiveness has been extensively studied. In CBT for depression, the therapist works with the client to identify negative thoughts and beliefs that are contributing to their depression. The therapist then helps the client to reframe these negative thoughts and beliefs in a more positive and realistic way. The therapist also works with the client to identify and engage in activities that bring pleasure and a sense of accomplishment. CBT for depression typically involves 12 to 16 weekly sessions and has been found to be as effective as medication in treating depression.
Anxiety Disorders
CBT is also a first-line treatment for anxiety disorders, including generalized anxiety disorder (GAD), panic disorder, social anxiety disorder, and specific phobias. In CBT for anxiety disorders, the therapist helps the client to identify and challenge negative thoughts and beliefs that contribute to their anxiety. The therapist also teaches the client relaxation techniques to manage their physical symptoms of anxiety, such as rapid heartbeat and shortness of breath. Exposure therapy is often used to help the client face their fears gradually, leading to desensitization and decreased anxiety over time. CBT for anxiety disorders typically involves 12 to 16 weekly sessions and has been found to be as effective as medication in treating anxiety disorders.
Obsessive-Compulsive Disorder (OCD)
CBT is a first-line treatment for OCD, which is characterized by recurrent, unwanted thoughts and repetitive behaviors. In CBT for OCD, the therapist helps the client to identify and challenge their obsessive thoughts and compulsive behaviors. The therapist also helps the client to develop alternative coping strategies, such as distraction techniques and mindfulness, to manage their anxiety and urge to perform compulsive behaviors. Exposure and response prevention (ERP) is often used to help the client face their fears gradually and resist the urge to perform compulsive behaviors, leading to desensitization and decreased anxiety over time. CBT for OCD typically involves 16 to 20 weekly sessions and has been found to be as effective as medication in treating OCD.
Post-Traumatic Stress Disorder (PTSD)

CBT is a first-line treatment for PTSD, which is a mental health disorder that can occur after experiencing or witnessing a traumatic event. In CBT for PTSD, the therapist helps the client to identify and challenge negative thoughts and beliefs about the traumatic event. The therapist also teaches the client relaxation techniques to manage their physical symptoms of anxiety and arousal, such as flashbacks and hypervigilance. Exposure therapy and cognitive restructuring are often used to help the client face their traumatic memories and develop more adaptive coping strategies. CBT for PTSD typically involves 12 to 16 weekly sessions and has been found to be as effective as medication in treating PTSD.
Eating Disorders
CBT is an effective treatment for eating disorders, including anorexia nervosa, bulimia nervosa, and binge-eating disorder. In CBT for eating disorders, the therapist helps the client to identify and challenge negative thoughts and beliefs about their body image and eating behaviors. The therapist also helps the client to develop a more positive and realistic self-image and healthy eating habits. Exposure therapy and cognitive restructuring are often used to help the client face their fears and develop more adaptive coping strategies. CBT for eating disorders typically involves 16 to 20 weekly sessions and has been found to be as effective as medication in treating eating disorders.
Substance Use Disorders

CBT is an effective treatment for substance use disorders, including alcohol and drug addiction. In CBT for substance use disorders, the therapist helps the client to identify and challenge negative thoughts and beliefs about their substance use. The therapist also helps the client to develop alternative coping strategies to manage their cravings and triggers, such as stress management techniques and healthy leisure activities. Exposure therapy and cognitive restructuring are often used to help the client face their fears and develop more adaptive coping strategies. CBT for substance use disorders typically involves 12 to 16 weekly sessions and has been found to be as effective as medication in treating substance use disorders.
Personality Disorders
CBT is also an effective treatment for personality disorders, including borderline personality disorder and narcissistic personality disorder. In CBT for personality disorders, the therapist helps the client to identify and challenge negative thoughts and beliefs that contribute to their maladaptive behaviors and interpersonal difficulties. The therapist also helps the client to develop more adaptive coping strategies, such as emotion regulation and interpersonal effectiveness skills. Cognitive restructuring and behavioral activation are often used to help the client develop more positive and adaptive patterns of thinking and behavior. CBT for personality disorders typically involves 20 to 24 weekly sessions and has been found to be effective in reducing symptoms and improving functioning.
Other Mental Health Conditions
CBT has also been found to be effective in treating other mental health conditions, such as insomnia, chronic pain, and somatic symptom disorder. In CBT for insomnia, the therapist helps the client to identify and challenge negative thoughts and beliefs about sleep and teaches them relaxation techniques to improve sleep hygiene. In CBT for chronic pain, the therapist helps the client to develop more adaptive coping strategies to manage their pain and improve their quality of life. In CBT for somatic symptom disorder, the therapist helps the client to identify and challenge their beliefs about their physical symptoms and develop more adaptive ways of coping.
Limitations of CBT
While CBT has been found to be effective in treating a wide range of mental health conditions, it does have some limitations. One limitation is that it may not be effective for everyone, as individual differences and preferences can affect treatment outcomes. Additionally, CBT requires active participation and effort from the client, which may be challenging for some individuals with severe mental health conditions or cognitive impairments.
Another limitation of CBT is that it may not address underlying biological or environmental factors that contribute to mental health conditions. In some cases, medication or other treatments may be necessary in addition to or instead of CBT.
Finally, access to CBT can be limited due to factors such as cost, availability, and stigma surrounding mental health treatment. However, there are resources available, such as online CBT programs and community mental health clinics, that can help to overcome these barriers.
Conclusion
CBT is a highly effective treatment for a wide range of mental health conditions, including depression, anxiety disorders, OCD, PTSD, eating disorders, substance use disorders, and personality disorders. In CBT, the therapist helps the client to identify and challenge negative thoughts and beliefs that contribute to their mental health symptoms and teaches them more adaptive coping strategies. While CBT has some limitations, it has been found to be as effective as medication in treating many mental health conditions and can help to improve the quality of life for individuals struggling with mental health issues. If you or someone you know is struggling with a mental health condition, consider reaching out to a mental health professional to learn more about CBT and other treatment options.
References:
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). American Psychiatric Publishing.
Beck, A. T. (1976). Cognitive therapy and the emotional disorders. Penguin.
Cuijpers, P., Sijbrandij, M., Koole, S. L., Andersson, G., Beekman, A. T., & Reynolds, C. F. (2013). The efficacy of psychotherapy and pharmacotherapy in treating depressive and anxiety disorders: A meta-analysis of direct comparisons. World Psychiatry, 12(2), 137–148.
Hofmann, S. G., Asnaani, A., Vonk, I. J. J., Sawyer, A. T., & Fang, A. (2012). The efficacy of cognitive behavioral therapy: A review of meta-analyses. Cognitive Therapy and Research, 36(5), 427–440.
Hollon, S. D., DeRubeis, R. J., Shelton, R. C., Amsterdam, J. D., Salomon, R. M., O’Reardon, J. P., Lovett, M. L., Young, P. R., Haman, K. L., Freeman, B. B., & Gallop, R. (2005). Prevention of relapse following cognitive therapy vs medications in moderate to severe depression. Archives of General Psychiatry, 62(4), 417–422.
Miklowitz, D. J., Otto, M. W., Frank, E., Reilly-Harrington, N. A., Kogan, J. N., Sachs, G. S., Thase, M. E., & Calabrese, J. R. (2007). Intensive psychosocial intervention enhances functioning in patients with bipolar depression: Results from a 9-month randomized controlled trial. American Journal of Psychiatry, 164(9), 1340–1347.
Pilling, S., Bebbington, P., Kuipers, E., Garety, P., Geddes, J., Orbach, G., & Morgan, C. (2002). Psychological treatments in schizophrenia: I. Meta-analysis of family intervention and cognitive behaviour therapy. Psychological Medicine, 32(5), 763–782.

