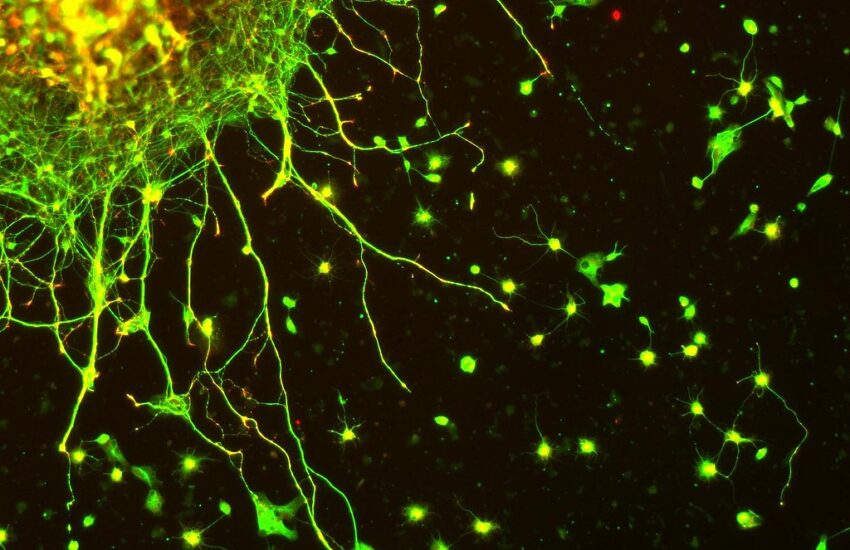
In the fall of 2007, I took a course at Georgetown University called Sense & Perception, taught by Professor Benjamin Fiore-Walker. The class didn’t just teach me something new. It rewired how I thought about the mind altogether. We spent weeks dissecting the neural machinery behind vision, hearing, and touch, learning how raw sensory data transforms into conscious experience. The material was dense, often frustrating, but it hammered home a fundamental truth: perception isn’t an abstract, disembodied process. It’s built on neurons firing, synapses transmitting, and ions flowing. Thus, the mind is inextricably physical.
That realization stuck with me. Over the years, as I delved deeper into psychology and neuroscience, I kept circling back to the idea that mental health must be grounded in biology. Not just neurotransmitters, but the broader biochemical environment of the brain. Then, while researching excess iron, I stumbled upon chelation therapy. At first, it seemed like a fringe concept, something relegated to heavy metal toxicity cases. But the more I read, the more I realized how profoundly metals influence cognition and emotion. Zinc, copper, iron, magnesium: they aren’t just passive elements. They shape neural function in ways we are only beginning to understand.
This led me to develop the concept of Neurometallics, which I define as an approach that examines how metal ions influence brain function and explores ways to recalibrate these essential elements for treating mental health conditions. The core premise is simple yet radical: many mental health conditions and neurological diseases stem from disruptions in metal homeostasis and correcting these imbalances should be the first line of intervention, not an afterthought.
The Rising Tide of Metal Dysregulation
When I first began diving into this research, I was struck by how metals accumulate in our bodies over time. It’s a process with profound implications for neurological health (Hare et al., 2013). What fascinated me most was discovering that some metals like iron and copper that are essential for physiological functions in trace amounts become neurotoxic when their delicate homeostasis is disrupted (Bush, 2003; Ward et al., 2014). Others, such as lead and mercury, have no biological role and are purely harmful, yet remain pervasive environmental contaminants (Caban-Holt et al., 2014). The body’s ability to maintain proper metal balance becomes increasingly compromised with age, leading to dysregulation that parallels the trajectory of neurological decline (Zatta et al., 2009).
Take zinc deficiency, for instance. I was fascinated by its consistent link to depression and cognitive impairment in clinical studies, with research demonstrating that depressed patients exhibit low zinc concentrations in serum that normalizes following successful antidepressant treatment (Nowak et al., 2011). Conversely, excess copper has been associated with anxiety and schizophrenia-like symptoms, and studies show that copper can accumulate in synaptic spaces where it disrupts neurotransmitter metabolism (Snyder, 2021; Schroder et al., 2019).
But here’s what really got my attention: how closely these metal imbalances mirror the progression of mental health disorders across the lifespan. Psychiatric conditions often emerge during adolescence or early adulthood, periods characterized by hormonal fluctuations that significantly affect metal metabolism (Davis, 2015). Later in life, neurodegenerative diseases like Alzheimer’s and Parkinson’s are marked by pathological iron and copper accumulation in specific brain regions (Ward et al., 2014; Zhu et al., 2023). Recent Mendelian randomization studies have established causal relationships between subcortical iron levels and major psychiatric disorders, with lower iron in the left substantia nigra increasing risk for major depressive disorder and schizophrenia (Zhu et al., 2023). These consistent patterns across diverse neuropsychiatric conditions made me wonder: could metal dysregulation be more than coincidental? Could it be causal?
Metals and Mental Illness: The Evidence So Far
When I started exploring the connection between metals and mental health, I expected to find only limited research linking heavy metal toxicity to neurological symptoms. What I discovered instead blew me away. There’s a substantial body of evidence demonstrating how essential metals (the very elements our brains depend on) can become pathological when their regulatory mechanisms fail (Bush, 2013; Nakagawa & Chiba, 2022). This isn’t merely about toxicity; it’s about subtle dysregulation that may underlie many common psychiatric disorders through mechanisms including oxidative stress, neuroinflammation, and disrupted neurotransmission (Nowak et al., 2011; Bush, 2013).
Lithium is perhaps the most striking example. I actually recalled first learning about its usage in my abnormal psychology course. It’s a simple metal that remains psychiatry’s most effective treatment for bipolar disorder, despite decades of research into synthetic alternatives (Malhi et al., 2013). The more I dug into the research, the more I realized how lithium operates through multiple mechanisms: stabilizing neuronal membranes, influencing circadian rhythms by interacting with key enzymes, and even mimicking magnesium in certain biochemical pathways (Manji et al., 1999; Malhi et al., 2013). Recent research suggests lithium may exert its therapeutic effects by acting on insulin signaling pathways, particularly the PI3K/Akt pathway, which aligns with emerging evidence that energy dysregulation represents a core deficit in bipolar disorder (Malhi et al., 2013). The fact that this elemental metal can so profoundly stabilize mood regulation reinforced my belief that inorganic elements play active, dynamic roles in mental health through complex cellular signaling networks.
The copper-zinc relationship presented another fascinating case study that kept me reading late into the night. These two metals exist in a carefully regulated balance throughout the body, but particularly in the brain where their ratio is critical for proper neuronal function (Shaflender, 2018; Schroder et al., 2019). When this balance shifts toward excess copper, we observe consequences that mirror several psychiatric symptoms. Research has demonstrated that copper can overstimulate certain receptors while inhibiting the conversion of dopamine to norepinephrine, creating a neurochemical environment that resembles anxiety disorders or even schizophrenia (Snyder, 2021; Schroder et al., 2019). A meta-analysis revealed increased copper and decreased zinc concentrations in the blood of schizophrenia patients, suggesting that ceruloplasmin-ferroxidase malfunction could play a role in this imbalance (Schroder et al., 2019). Meanwhile, zinc deficiency appears to weaken the brain’s resilience to stress and impair neurogenesis in the hippocampus, a region critically involved in mood regulation (Nowak et al., 2011). Clinical trials have shown that zinc supplementation produces significant antidepressant effects when added to standard treatments, with improvements measurable on standardized depression scales (Ranjbar et al., 2013).
Iron’s role in mental health revealed yet another layer of complexity that kept drawing me deeper into this research. Essential for oxygen transport and myelin production, iron becomes problematic when it accumulates in vulnerable brain regions like the substantia nigra or hippocampus (Ward et al., 2014; Zhu et al., 2023). Through what’s known as Fenton chemistry, excess iron generates highly reactive hydroxyl radicals that damage neurons through oxidative stress (Smith et al., 1997). This process appears central to neurodegenerative diseases like Parkinson’s and Alzheimer’s, where iron accumulation has been directly visualized in the pathological hallmark lesions of these conditions (Bush, 2003; Ward et al., 2014). Recent research has demonstrated that this iron is redox-active and able to participate in in situ oxidation, readily catalyzing hydrogen peroxide-dependent oxidative damage (Smith et al., 1997). Furthermore, iron accumulation may contribute to treatment-resistant depression when it builds up in the basal ganglia, with a 2025 Mendelian randomization study establishing causal relationships between regional brain iron levels and specific psychiatric disorders (Zhu et al., 2023).
The neurotoxicity of heavy metals like lead and mercury became equally compelling to me despite being better recognized. Even at low exposure levels, these metals interfere with crucial neurological processes through multiple mechanisms (Caban-Holt et al., 2014). Lead disrupts calcium signaling pathways that are essential for synaptic plasticity, while mercury binds to and disables critical antioxidant enzymes, leaving brain cells vulnerable to oxidative damage (Yuan & Atchison, 2012). Mercury has been shown to disrupt glutamate signaling, simultaneously enhancing its release from pre-synaptic terminals while hindering uptake by astrocytes, creating neuronal excitotoxicity (Yuan & Atchison, 2012). The cognitive and behavioral consequences (ranging from ADHD-like symptoms in children to depression and memory problems in adults) suggest these metals may be silent contributors to many cases currently classified as idiopathic mental illness (Caban-Holt et al., 2014).
What excites me most are the emerging therapeutic approaches targeting metal homeostasis. The cognitive improvements observed with alpha-lipoic acid administration in Alzheimer’s disease patients are particularly promising, with one 48-month follow-up study showing dramatically slower disease progression in treated patients compared to historical controls on standard therapy (Hager et al., 2008). Similarly, the mood benefits of zinc supplementation in depression have been demonstrated in randomized clinical trials, with significant improvements in depression scores when zinc is added to standard antidepressant treatment (Ranjbar et al., 2013). The protective effects of iron chelation in models of neurodegeneration point toward a new paradigm in mental health treatment (Bush, 2013). We’re not just managing symptoms but potentially addressing underlying biochemical disturbances that may represent root causes of neuropsychiatric disorders.
A Proposal for a New Approach
Given this evidence, I believe now is the time to test Neurometallics in a structured clinical trial. The goal would be to evaluate whether a combination of safe metals and metal-modulating compounds (such as R-alpha-lipoic acid, L-carnosine, glycine, and sulforaphane) can improve symptoms in patients with mood disorders, schizophrenia, or neurodegenerative conditions. Unlike traditional psychiatric treatments, which often focus on symptom management, this approach would aim to correct root-cause imbalances first.
Of course, this isn’t about eliminating existing therapies. It’s about adding a missing layer to mental health care. Before adjusting serotonin or dopamine, we should ask: Are this patient’s metals in balance? Are they deficient in zinc, overloaded with copper, or accumulating iron? Answering these questions could lead to more precise, effective treatments.
The Path Forward
The science of Neurometallics is still young, and skepticism is warranted. We need rigorous studies to confirm which metal imbalances matter most and how best to address them. But the preliminary data is compelling enough to warrant serious investigation. If we accept that mental health is fundamentally biological, then it’s only logical to explore the role of metals (one of the most basic, yet overlooked, components of brain function).
A clinical trial would be the next critical step. By systematically testing metal-modulating interventions, we could move beyond anecdotal reports and establish evidence-based protocols. Until then, I’ll keep advocating for this perspective, not as a rejection of current treatments, but as a necessary evolution in how we understand and treat the mind.
In the end, the mind isn’t separate from the body. It is the body. And if we want to heal it, we have to start with the fundamentals.
References
Bush, A. I. (2003). The metallobiology of Alzheimer’s disease. Trends in Neurosciences, 26(4), 207-214.
Bush, A. I. (2013). Editorial: Metals and neurodegeneration: restoring the balance. Frontiers in Aging Neuroscience, 7, 127.
Caban-Holt, A., Mattingly, M., Cooper, G., & Schmitt, F. A. (2014). Pb neurotoxicity: neuropsychological effects of lead toxicity. BioMed Research International, 2014, 840547.
Davis, M. (2015). Hormones and the adolescent brain. BrainFacts/SfN.
Hager, K., Kenklies, M., McAfoose, J., Engel, J., & Münch, G. (2008). Lipoic acid as an anti-inflammatory and neuroprotective treatment for Alzheimer’s disease. Advanced Drug Delivery Reviews, 60(13-14), 1463-1470.
Hare, D., Ayton, S., Bush, A., & Lei, P. (2013). A delicate balance: Iron metabolism and diseases of the brain. Frontiers in Aging Neuroscience, 5, 34.
Malhi, G. S., Tanious, M., Das, P., Coulston, C. M., & Berk, M. (2013). Potential mechanisms of action of lithium in bipolar disorder. CNS Drugs, 27(2), 135-153.
Manji, H. K., Bebchuk, J. M., Moore, G. J., Glitz, D., Hasanat, K. A., & Chen, G. (1999). Molecular mechanisms underlying mood stabilization in manic-depressive illness: the phenotype challenge. American Journal of Psychiatry, 156(10), 1506-1514.
Nakagawa, K., & Chiba, K. (2022). The relationships among metal homeostasis, mitochondria, and locus coeruleus in psychiatric and neurodegenerative disorders: potential pathogenetic mechanism and therapeutic implications. Neuropsychopharmacology Reports, 42(2), 204-217.
Nowak, G., Siwek, M., Dudek, D., Zieba, A., & Pilc, A. (2011). The role of zinc in neurodegenerative inflammatory pathways in depression. Progress in Neuro-Psychopharmacology and Biological Psychiatry, 35(3), 693-701.
Ranjbar, E., Kasaei, M. S., Mohammad-Shirazi, M., Nasrollahzadeh, J., Rashidkhani, B., Shams, J., … & Mostafavi, S. A. (2013). Effects of zinc supplementation in patients with major depression: a randomized clinical trial. Iranian Journal of Psychiatry, 8(2), 73-79.
Schroder, N., Figueiredo, L. S., & de Lima, M. N. (2019). Cortical biometals: changed levels in suicide and with mood disorders. Neurochemistry International, 125, 10-19.
Shaflender, M. (2018). Copper: The key mineral for emotional, hormonal & mental health. LinkedIn.
Smith, M. A., Harris, P. L., Sayre, L. M., & Perry, G. (1997). Iron accumulation in Alzheimer disease is a source of redox-generated free radicals. Proceedings of the National Academy of Sciences, 94(18), 9866-9868.
Snyder, C. (2021). Copper overload/toxicity & brain disorders. Holistic Psychiatry Podcast.
Ward, R. J., Zucca, F. A., Duyn, J. H., Crichton, R. R., & Zecca, L. (2014). The role of iron in brain ageing and neurodegenerative disorders. The Lancet Neurology, 13(10), 1045-1060.
Yuan, Y., & Atchison, W. D. (2012). Mercury-induced toxicity of rat cortical neurons is mediated through N-methyl-D-aspartate receptors. NeuroReport, 23(14), 838-844.
Zatta, P., Drago, D., Bolognin, S., & Sensi, S. L. (2009). Metal dyshomeostasis in the brain: a possible cause for several neurodegenerative disorders. Neurobiology of Disease, 36(1), 1-10.
Zhu, W., Zheng, H., Shao, X., Wang, W., Yao, Q., & Li, Z. (2023). Brain iron homeostasis and mental disorders. Brain Research Bulletin, 193, 1-13.