Mental health stigma prevents millions from seeking help. Understand its roots, recognize its impact, and learn how we can collectively create a more compassionate world. I’ll never forget the moment my father referred to his new antidepressant medication as his “blood pressure pills” at a family gathering. When I asked him about it later, he admitted, “It’s easier than explaining the truth.” That quiet confession revealed more about the power of stigma than any textbook ever could. His fear of judgment ran so deep that he’d rather conceal part of his healthcare than face potential misunderstanding. This is how stigma operates, not through dramatic confrontations, but through whispered apologies, concealed medications, and carefully crafted lies that eventually make people feel alienated from their own experiences.
Mental health stigma manifests in multiple dimensions, each with devastating consequences. Public stigma involves the negative attitudes and beliefs that society holds about mental illness, the assumption that people with depression are “lazy,” that those with anxiety should “just relax,” or that individuals with schizophrenia are “dangerous.” These stereotypes permeate our language, our media, and our cultural narratives, creating an environment where mental health conditions are moralized rather than medicalized. I’ve watched brilliant colleagues hesitate to take mental health days while casually discussing physical ailments, revealing how we’ve normalized one type of suffering while shrouding another in shame.
Self-stigma often proves even more damaging than public judgment. This internalized shame leads individuals to absorb negative stereotypes and apply them to themselves—believing they’re “weak” for needing therapy or “broken” because they struggle with mental health. I’ve sat with therapy clients who expressed more self-judgment about their anxiety symptoms than their cancer diagnoses, illustrating how effectively stigma teaches us to condemn our own minds. This self-stigma creates what psychologists call the “why try” effect—if someone believes they’re incompetent or unworthy due to their mental health condition, they’re less likely to pursue relationships, opportunities, or treatment.
The structural dimension of stigma often goes unrecognized but creates tangible barriers to care. Insurance plans that offer limited mental health coverage, workplaces without adequate mental health policies, and healthcare systems that separate mental and physical treatment all institutionalize the message that mental health matters less. I’ve reviewed insurance policies that covered 30 physical therapy sessions but only 12 mental health sessions annually, a numerical value judgment that speaks volumes about our priorities. These systemic barriers disproportionately affect marginalized communities, compounding stigma with disparities in access and quality of care.
The language we use either reinforces or reduces stigma. Terms like “crazy,” “psycho,” or “deranged” seem harmless to some but perpetuate negative associations for others. I’ve watched people flinch at casual references to “OCD cleaning” or “bipolar weather,” their pain invisible to those who don’t understand how metaphorical use of clinical terms minimizes real suffering. Conversely, I’ve seen relief wash over someone when they hear a supervisor say “I’ve been in therapy too” or a friend ask “How’s your mental health been?” with the same ease they’d ask about physical health.
Media representation plays a powerful role in shaping perceptions. For decades, television and film disproportionately linked mental illness with violence, creating false associations that persist despite evidence that people with mental health conditions are more likely to be victims than perpetrators. The recent shift toward more nuanced portrayals—showing characters managing conditions while living full lives, helps normalize the reality that mental health challenges exist on a spectrum and don’t define a person’s entire identity.
Combating stigma requires moving beyond awareness to action. Educational initiatives must address mental health literacy—teaching people to recognize symptoms, understand treatments, and respond supportively. Workplace policies need to provide genuine mental health support through Employee Assistance Programs, flexible scheduling for therapy appointments, and leadership that models vulnerability. I’ve seen executives share their mental health journeys with teams, creating permission for others to prioritize self-care without fear of professional consequences.
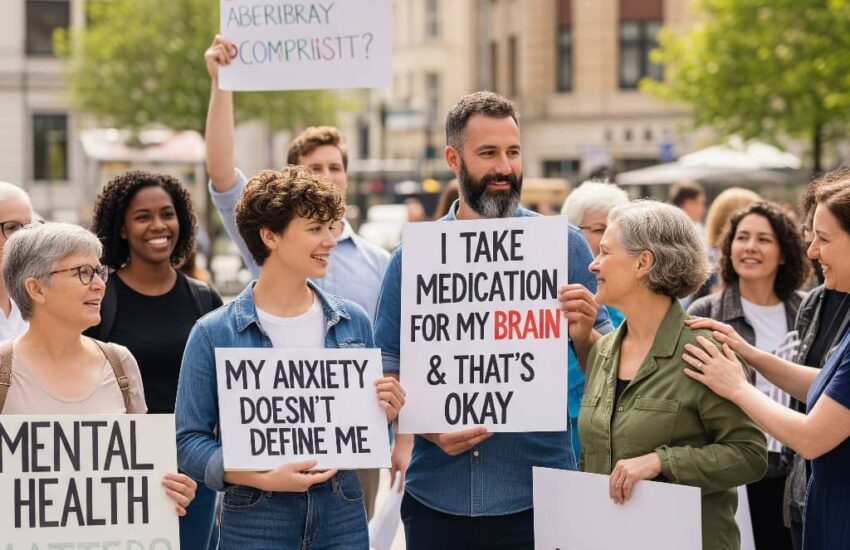
Personal storytelling remains among the most powerful tools against stigma. When people share their experiences with mental health challenges, they transform abstract statistics into human connections. I’ve watched support groups where someone saying “me too” instantly dissolves isolation that lasted years. These stories don’t need to be dramatic, sometimes the most impactful moments come from someone simply mentioning they take medication or see a therapist, normalizing these choices through casual visibility.
The relationship between stigma and treatment avoidance creates a dangerous cycle. Fear of judgment prevents people from seeking help, which allows conditions to worsen, which in turn reinforces the belief that mental health challenges are insurmountable. Breaking this cycle requires creating multiple pathways to care—from traditional therapy to peer support groups, crisis text lines to community workshops. I’ve seen churches host mental health first aid training, schools implement social-emotional learning curricula, and barbershops train stylists to recognize signs of depression in their clients—all innovative approaches that meet people where they are.
Cultural competence is essential for addressing stigma in diverse communities. Different cultures express and interpret mental health symptoms differently, and what constitutes stigma varies across groups. Some communities experience mental health challenges primarily through physical symptoms, while others emphasize spiritual dimensions. Effective anti-stigma work must respect these differences while providing culturally responsive care. I’ve worked with clinicians who incorporate traditional healing practices alongside evidence-based treatments, honoring whole persons rather than just diagnoses.
The economic argument against stigma often gets overlooked. Mental health conditions cost the global economy approximately $1 trillion annually in lost productivity, a figure that doesn’t account for the human suffering behind it. Workplace mental health programs typically show return on investment between $2-4 for every dollar spent, making stigma reduction not just ethically right but economically smart. Forward-thinking companies now track mental health metrics alongside other business indicators, recognizing that psychological safety drives innovation and performance.
Ultimately, reducing stigma requires recognizing that mental health exists on a continuum that includes us all. We all have mental health, just as we all have physical health, some days better, some days worse. Creating a world where people can seek help without shame means building communities where we check on each other’s emotional well-being as naturally as we discuss the weather, where therapy is viewed as maintenance rather than repair, and where taking medication for your brain carries no more judgment than taking insulin for your pancreas. This isn’t a distant fantasy, it’s a future we create through everyday choices to speak openly, listen compassionately, and reject the silence that stigma requires.
References
Ahad, A. A. (2023). Understanding and addressing mental health stigma: A multifaceted challenge across cultures. *Frontiers in Psychiatry*. https://pmc.ncbi.nlm.nih.gov/articles/PMC10220277/
This comprehensive review highlights how stigma delays treatment, reduces quality of life, and affects patients, families, healthcare providers, and society at large.
Depression and Bipolar Support Alliance Oklahoma. (2024, January 4). Primary barriers to recovery for persons with mental illness. https://dbsaok.org/primary-barriers-to-recovery-for-persons-with-mental-illness/
Explores stigma-related barriers including self-stigma, discrimination, social isolation, and lack of access to quality care that impede recovery.
da Silva, A. G. (2020). The impact of mental illness stigma on psychiatric emergency care. *Frontiers in Psychiatry*. https://www.frontiersin.org/journals/psychiatry/articles/10.3389/fpsyt.2020.00573/full
Discusses how stigma affects emergency mental health treatment and leads to delays in care and worsened patient outcomes.
Gardner, V. M. (2025, August 14). The impact of stigma on mental health: Barriers, consequences, and solutions. Henry Ford Behavioral Health. https://www.henryford.com/mimind/news/blog/the-impact-of-stigma-on-mental-health
Examines public, self, structural, and healthcare provider stigma and their effects on treatment adherence and recovery.
Wahl, O. F. (2012). Stigma as a barrier to recovery from mental illness. *Trends in Cognitive Sciences*, 16(1), 1-3. https://pubmed.ncbi.nlm.nih.gov/22153582/
Summarizes research on prejudice and discrimination as key obstacles to mental health recovery, emphasizing the need to reduce stigma through education and policy.