Learn about Transcranial Magnetic Stimulation, a non-invasive treatment for depression and anxiety. Discover how TMS works, its benefits, and what to expect from this innovative therapy.
In the landscape of mental health treatment, there often comes a point where talk therapy and standard medications feel like a path that has run its course. For millions living with treatment-resistant depression or severe anxiety, this impasse can feel like a final verdict.
But a different kind of path exists, one that bypasses the digestive system and the conscious narrative to speak directly to the brain’s neural circuitry. This path is Transcranial Magnetic Stimulation, a non-invasive, FDA-approved therapy that uses targeted magnetic pulses to gently “reset” brain activity in key regions implicated in mood regulation. TMS represents not a last resort, but a scientifically-grounded alternative for those seeking a different biological approach to healing.
TMS operates on a clear, elegant principle. While the brain uses electrical impulses to communicate, it also responds to magnetic fields. A TMS device contains an electromagnetic coil that is placed against the patient’s scalp, typically targeting the left dorsolateral prefrontal cortex, an area often underactive in depression.
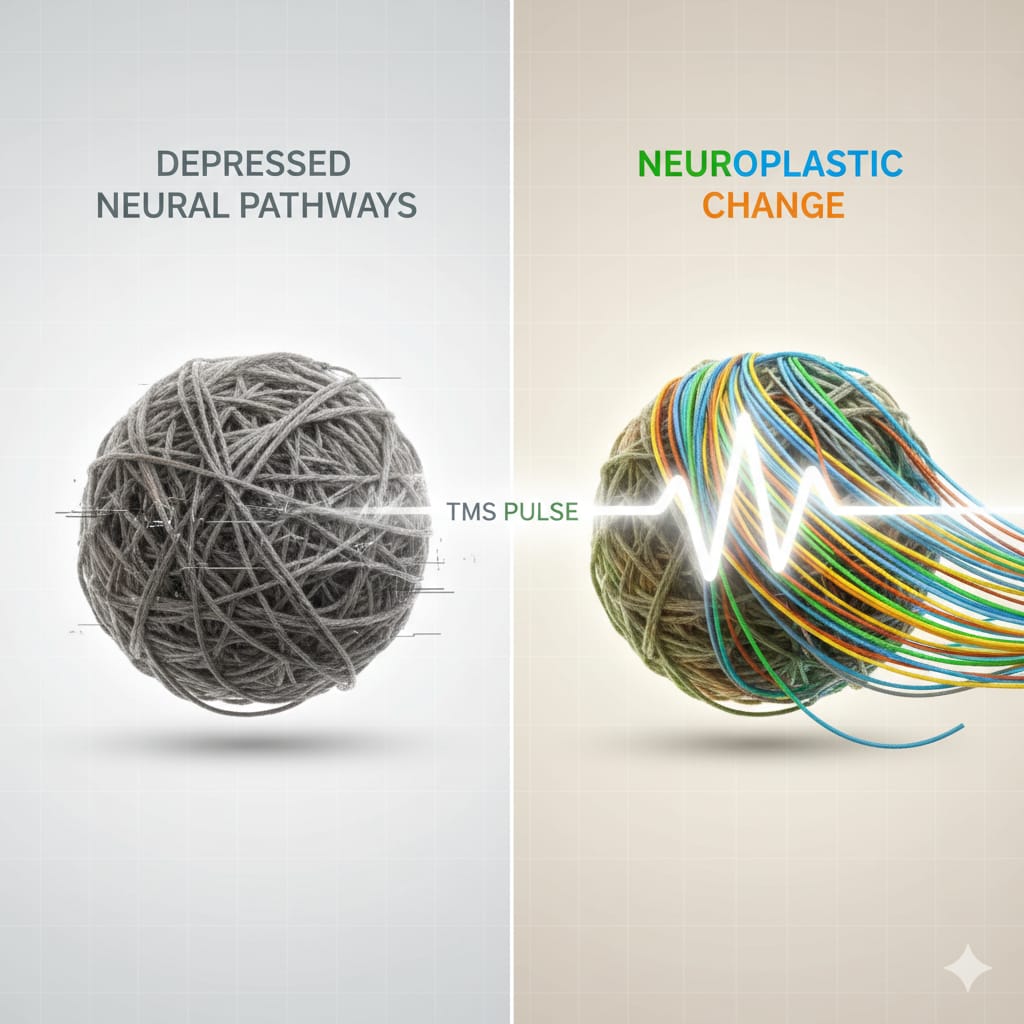
When activated, the coil generates brief, focused magnetic pulses that pass painlessly through the skull and induce a small electrical current in the targeted brain tissue. This current stimulates neurons, encouraging them to fire and, over repeated sessions, promoting neuroplasticity, the brain’s ability to form new, healthier connections and pathways.
Think of it as a gentle, precise tuning of a specific brain network that has fallen out of rhythm, helping to restore more balanced and resilient patterns of activity.
The treatment protocol is methodical and conducted in an outpatient setting. A patient sits in a comfortable chair, awake and alert, for a session lasting about 20-40 minutes. During the first appointment, the physician performs a “mapping” procedure to determine the precise location and optimal stimulation strength for the individual’s brain, finding their personal treatment coordinates.
A typical course involves daily sessions, five days a week, for four to six weeks. Patients often read, listen to music, or simply relax during the procedure, which is notable for its lack of systemic side effects. The most common sensation is a light tapping on the scalp, and there is no need for anesthesia or recovery time; patients can drive themselves home and resume normal activities immediately.
The clinical profile of TMS is what makes it a significant option. It is FDA-approved specifically for Major Depressive Disorder in patients who have not achieved satisfactory improvement from one or more antidepressant medications. It is also FDA-cleared for Obsessive-Compulsive Disorder and holds promise for generalized anxiety disorder and other conditions, often used “off-label” by experienced providers.
Its primary advantage is its favorable side effect profile. Unlike many medications, TMS does not cause weight gain, sexual dysfunction, or drowsiness. The most common side effects are mild scalp discomfort or headache during initial treatments, which typically fade.
The risk of seizure is extremely low (far less than 0.1%) and is carefully managed through screening and protocol adherence. For many, this targeted approach offers relief without the broad systemic trade-offs of pharmacotherapy.
TMS is not a standalone miracle cure; it is a powerful biological intervention best integrated into a comprehensive treatment plan. It does not teach coping skills or process trauma, so it is often combined with psychotherapy to help patients build upon the newfound stability it can provide.
The goal is to lift the heavy, physiological weight of depression or anxiety enough for a person to fully engage in the work of therapy and life. For those who have felt stuck in the exhausting cycle of medication trials, TMS offers a tangible sense of hope, a chance to intervene directly at the source of dysregulation.
It stands as a testament to the evolving understanding of mental health, proving that healing can come not only from changing our thoughts or our chemistry, but sometimes, from gently encouraging our brain to rediscover its own healthy rhythm.
References
Centers for Medicare & Medicaid Services. (2023). *Transcranial magnetic stimulation coverage criteria for depression*. U.S. Department of Health and Human Services. Retrieved from CMS Local Coverage Determination
Cole, E. J., et al. (2020). *Efficacy of transcranial magnetic stimulation in treatment-resistant depression with comorbid anxiety*. *Journal of Clinical Psychiatry, 81*(1), 22m14571. https://doi.org/10.4088/JCP.22m14571
Perera, T., George, M. S., Grammer, G., et al. (2020). *Use of transcranial magnetic stimulation for depression*. *Current Behavioral Neuroscience Reports, 7*(4), 243-252. https://doi.org/10.1007/s40473-020-00215-y
Mayo Clinic. (2023, April 6). *Transcranial magnetic stimulation*. Retrieved from https://www.mayoclinic.org/tests-procedures/transcranial-magnetic-stimulation/about/pac-20384625
Stanford Medicine. (2021, October 28). *Experimental depression treatment is nearly 80% effective*. Retrieved from https://med.stanford.edu/news/all-news/2021/10/depression-treatment.html